How Medical Research Failed Your Mother
90,000 women died preventable deaths because a flawed study convinced them their life-saving medication would kill them, and because the medical establishment has never prioritized getting women’s health right.
Reading Time: 5 minutes
Like all transformative change, the transition from child to adult can be painful. Yet, the cause of mood swings, irritability, anxiety, or sadness isn’t always obvious; that’s because it’s caused by an invisible, ever-shifting, and tedious balance of hormones. While most of us have been focused on our own evolution, our own mothers have been quietly experiencing a change of their own: menopause.
Comparable to puberty in reverse, menopause is the process by which a woman’s body stops producing the necessary hormones to support menstruation—a painful and confusing transition that can take years. Hormones are largely responsible for regulating your brain chemistry, emotions, stress responses, energy, and sleep. When hormones are going through dramatic or unexpected shifts, women can be left with brain fog, mood swings, and emotional instability that can spiral into clinical depression. For some, it becomes a matter of life and death.
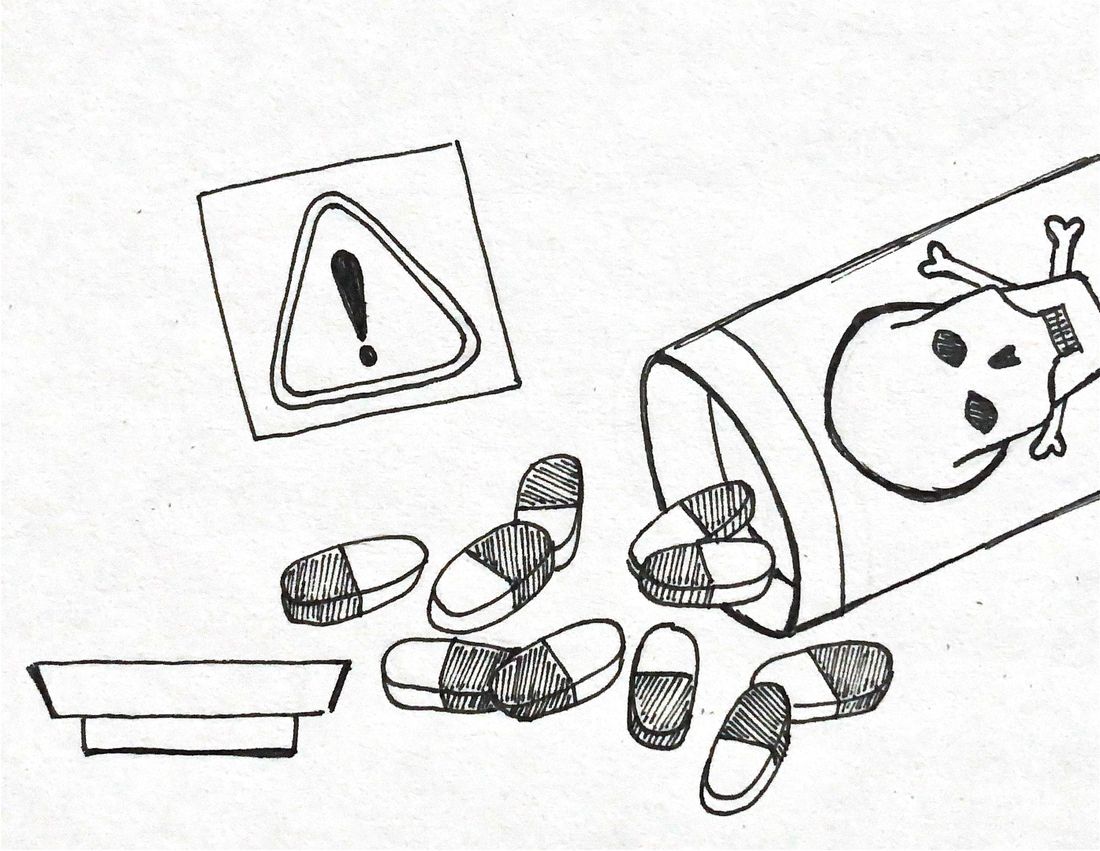
There are treatments that make this transition manageable, but for decades, an unfortunate stigma has bloomed over the use of hormone replacement therapy (HRT) drugs for women suffering from menopausal symptoms. This life-saving medication became taboo after a flawed but widely disseminated 2002 Women’s Health Initiative study, which sparked a panic that slammed the door shut on this effective treatment and cost thousands of women their lives.
The scientific community justified and propelled these women’s fears. The study reported that HRT usage was associated with a 26 percent increased risk in breast cancer. This number was shocking and frightening to the women who had relied on these drugs to stabilize their moods and lifestyles for years. Breast cancer is one of the leading causes of death in women, second only to lung cancer. It affects one in every eight women—a 26 percent increase would mean one in six. To most of these women, the chance seemed intolerable. Virtually overnight, HRT prescriptions plummeted by 46 percent in the US.
The study, however, was fundamentally flawed—and while its statistical manipulation may not have had malicious intentions, it reflected a severe level of carelessness. In reality, the true figure was one additional case per 1,000 women, numerically insignificant but inflated to sound like a 26 percent increase. Worse, the average participant in this study was 63 years old—more than a decade past typical menopause onset—making the study wholly irrelevant to the women who need HRT. The older women in the study already had elevated risks for heart disease and cancer due to their age, not necessarily their use of medication.
What got lost in the fear-mongering about marginal cancer risks was the very real, very deadly mental health crisis that untreated menopause can trigger. While menopause is often framed as a manageable inconvenience, its side effects cannot always be solved with time and patience. Menopause is rooted in the decline of estrogen, which disrupts bodily stress response and emotional regulation on a fundamental level. These hormonal fluctuations are linked to an array of psychiatric conditions, including anxiety, cognitive decline, and insomnia.
Recent research has revealed that the hormonal chaos of perimenopause and menopause creates one of the most emotionally vulnerable stages in a woman’s life. Women in the perimenopausal period face an almost sevenfold increase in risk of suicidal ideation and severe depression compared to women in the pre- or post-menopausal period. This increased risk occurs independently of underlying mood disorders, meaning even women with no history of depression can suddenly face suicidal thoughts during menopause.
After the study came out, a warning label on all packaging was mandated to reveal potential risks. “WARNING: probable endometrial cancer, cardiovascular disorders, dementia, and breast cancer,” one line read. It wasn’t until November 2025 that the Food and Drug Administration finally removed these misleading black box warnings, more than two decades after the data was found to be inaccurate.
After the release of the Women’s Health Initiative Study, distrust in HRT solidified; not just toward the medication itself, but menopause treatment as a whole. This fear-driven retreat from medication had horrifying consequences: research estimates as many as 91,610 women died prematurely as a result of menopausal side effects, including suicide, that HRT drugs could have helped prevent. The FDA’s admission came far too late for the women who died unnecessarily, for the thousands who took their own lives when proper treatment could have saved them had they not been irrationally afraid.
This was not an anomaly, but a predictable result of a medical research field that cuts corners when studying women’s health. Yes, the Women’s Health Initiative simply miscalculated the risk, but in doing so it reflected the broader structural bias in how women’s health is studied, funded, and applied. Throughout history, medical studies have generalized data collected from males and applied it to females despite profound biological differences. For decades, the Caucasian male was considered the ideal study population, while women were avoided because their fluctuating hormones were deemed inconvenient to accommodate. This complexity should have prompted rigorous study, not sidestepping. As a result, drugs are often approved with little understanding of how dosage, side effects, or long-term risks differ for female bodies. Women remain chronically underrepresented in clinical trials. Even when included, their results are often not analyzed separately by sex.
Pharmaceutical companies and citizens alike must acknowledge this public health crisis created by scientific carelessness and exacerbated through media hysteria. Women deserve doctors and scientists who understand that menopause without HRT treatment can drive them to suicide. They deserve access to safe and effective treatment without stigma. And moreover, they deserve an apology for two decades of preventable suffering they were put through.
The FDA’s 2025 decision is a start, but it is nowhere near enough. Preventing the next crisis requires systemic reform: expanding access to HRT medication, educating healthcare providers about the life-threatening risks of untreated menopause, and committing to undoing years of irrational fearmongering that has cost too many women their lives. To end misogyny in the medical field, misrepresentation must not be frowned upon as a cultural offense but as a scientific failure. Clinical trials should not be published or approved without sex-specific analysis and a clear understanding of their effects through life on both female and male bodies. Most importantly, pharmaceutical companies must be required to correct errors in real time when it matters most, not decades later.
Today, we know that women did not die because menopause is dangerous, but because precision is deemed optional when the patients are women. Our generation can be the turning point to transform a history of neglect into a future where women’s health is investigated with the same rigor as men’s.